
Journey of evolution of gadgetry in anaesthesiology
Anaesthesia, as known to the fraternity is an important part of surgery, as it enables patients to undergo procedures that lead to healthier and longer lives, safely without experiencing distress and pain. Anaesthesia was a mystery before the 19th century. The astronomical development that took place in the scientific world, with the invention of gadgets, during the last two centuries, contributed vastly to the concurrent development in the field of medicine. The advances in surgery mandated advances in anaesthesiology too. With electronics, internet and digital world taking us forward into the era of Artificial Intelligence, light years of advancement has been witnessed in the field in complex gadgets. We must understand and appreciate the work undertaken by our forefathers, as has always been and will be the stepping stones and inspiration for the next gadgetry invention to be added into our armamentarium.

The speciality of anaesthesia garnered recognition when WTG Morton first publicly demonstrated the use of inhaled ether as a surgical anaethetic in 1846.Many Scientists like Horace Wells, Crawford W. Long, a Georgia practitioner who claimed to have used nitrous oxide and ether as early as 1842, toyed with anesthetic agents and Charles Jackson, Morton’s Chemistry Professor, it was, however, Morton who first developed a novel delivery instrument to enable ether inhalation during an operation and perhaps thus, ushered the era of the use of gadgets in the practise of anaesthesia.1
For many years an anaesthesia machine was not used for providing anaesthesia to the patients until oxygen (O2) and nitrous oxide (N2O) were introduced as compressed gases in cylinders by the late 19th century, 1880. Invention of compressed gas cylinders was one of the most important developments in the field of medical practice. Oxygen and other gases were compressed and stored at high pressure in seamless containers constructed from hand-forged steel. A metal skeleton was required for mounting these cylinders.
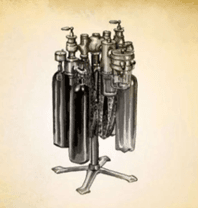
Dentist brothers, Charles K Teter and William C Teter patented the ‘Teter anaesthesia apparatus’ in 1902, which could provide O2, N2O, and Ether, and became the first machine to deliver all the three agents whish became the standard for all anesthesia machines for the next two decades
Dr. Frederic J. Cotton (1869-1938) and Dr. Walter Boothby (1880-1953) at the Boston City Hospital developed a similar apparatus and introduced its in 1911. They wanted a device that could provide an uninterrupted flow of anesthetics and oxygen, a visible indication of the rate of flow for both the nitrous oxide (N2O) and oxygen (O2), and the means to quickly and easily add ether vapor to the gas mixture.

On concurrent lines another apparatus was developed, the Gwathmey–Woolsey apparatus on the name of the scientists.
Dr. Henry E. G. Boyle (1875-1941), a leading English anesthetist, invented a nitrous oxide, oxygen and ether anesthesia machine in 1917. It was based on the design of the Gwathmey Apparatus, using a “bubble through” or “sight feed” vaporizer. This became widely known as the Boyle Bottle. The Boyle machine continued in production for over 50 years, while the Boyle Bottle became a standard feature of British anesthesia machines. The anesthetic agent, halothane (Fluothane) was introduced in Great Britain in 1955.


Dr. Karl Connell (1878-1941) introduced a line of closed circuit, multiple-gas anesthesia machines in the 1930s. These were among the first to have a built-in CO2 absorber. This series of machines also had ball-bearing gauges, called flow meters, to accurately display the rate of gases flowing to the patient.

In 1923, the pioneering anesthesiologist Dr. Ralph Waters incorporated a CO2 absorption system into an anesthesia circuit, beginning the practice of low-flow anesthesia and reuse of agent with the patient re-breathing his own scrubbed exhalations. In 1941, the “Coxeter-Mushin” circle absorber unit was incorporated in Boyle’s EMS model, however, known not to be a true circle system in that the soda lime container does not lie in the circle. The later was rectified only after efficiency was not proven around 1955.

However, a modern anaesthesia machine is incomplete without a vapouriser. The onus of development of which rests on Macintosh. In 1937, he along with Epstein, a physicist from Berlin, and other specialists in chemistry and physiology, designed what became known as the Oxford vaporizer. Another major advance was achieved in 1952, when Lucien Morris introduced a new vaporizer, the “Copper Kettle”, and was first manufactured by the Foregger company in the United States and became the vaporizer of choice for the administration of halothane.

With complexity and complications and law suits becoming increasingly problematic, safety issues ensued and thus reflected in delivery of accurate doses of anesthetics. A string of inventions, Goldman’s vapouriser (1959) for halothane, Rowbotham’s vapouriser, Oxford Miniature vapouriser (1960) followed hence.

With advances in delivery technology, the series of improvised developments ensued through the last half a century. They were temperature compensated, hence Tec series
Tec 2 (Ohmeda) halothane vapouriser: Launched in 1959, it can be called the first modern precision agent specific vapouriser. The earlier type, Mark 1 (Mk 1) was short-lived. By fixing a vapour control dial to the rotational ‘Barrel’ of Mk 1 (which caused practical problem) Mk 1 was upgraded to Tec 2.
Tec 3 vapouriser: It was introduced in the late 1960s due to drawbacks of the Tec 2 particularly the problems of the thymol causing operating spindle to stick, the pumping effect and the high concentration at low flows.
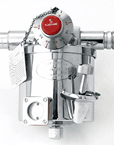
Tec 4 vapouriser: A vapouriser designed for ‘out-of-circuit’ use in continuous flow techniques of inhalation anaesthesia with built in temperature-compensated and pressure-compensated capabilities. Introduced in 1983 to overcome previous problems. with the safety interlock system and agent specific.
Tec 4, 5 and 7 being more technologically superior and confirming to set standardised safety sysytems. Aladin cassette vaporiser is in many ways similar to the other variable bypass vaporisers such as Tec 7 vaporisers. It a detachable cassette that serves as the vaporising chamber.


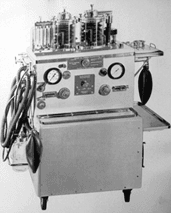
Another integral part of modern Anaesthesia machines are the ventilators. Mechanical ventilators were introduced into anesthetic practice in the early 1950s and quickly became standard components of anesthetic machines, within equipment such as the Blease Pulmoflator, the Engström apparatus, the Cape machine and the Barnet machine. It was an integrated manual ventilator for the application of positive pressure, associated with anesthetic vaporizers or nitrous oxide bottles.

The introduction of curare into clinical anesthetic practice, and the triumph of positive pressure ventilation over negative pressure ventilation in 1952, during the Copenhagen poliomyelitis epidemic boosted the acceptance of the ventilator in anesthetic machines. Thus, during the 1950s, in addition to the ventilator-equipped anesthesia apparatus described by Wilkinson, the Dräger company produced the “Dräger Pulmomat” in 1952, an additional unit to be connected to any Dräger anesthetic machine with a circle system eg. ‘Dräger Romulus’ model of anaesthesia machine.
Later, in 1959, the Spiromat 5000 anesthetic machine was designed as a combination of the Spiromat 4900 long-term ventilator and the Romulus anesthetic machine. From the 1960s, various Medical Products began incorporating ventilators into their anesthesia equipment. Since then, the ventilator has become an essential component of anesthetic machines. Today, with century long efforts poured in by mighty minds, we now possess anesthesia workstations, wherein incorporated are gas analyses along with vital monitoring system with display.

The anaesthesiologist is incomplete without his gadgets for airway management and manipulation.
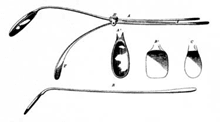
Benjamin Guy Babington presented his laryngoscope (he called it a ‘glottoscope’, which sometimes is referred to as the ‘glottiscope’) to the Hunterian Society in 1829 which consisted of a speculum to displace the tongue (a tongue depressor) and a system of mirrors to visualise the larynx, with sunlight for illumination.

Chevalier Jackson, Professor of Laryngology, Philadelphia, Pennsylvania, was the first to describe the combination of direct visualisation of the larynx with endotracheal intubation. In 1903 he designed his first laryngoscope, a U-shaped tubular instrument with a spatula and a tubal handle.
Henry Harrington Janeway, an American anaesthetist practising at Bellevue Hospital in New York in 1913, was the first anaesthetist to publish on direct laryngoscopy. In the same year, he designed a battery-powered laryngoscope, solely dedicated for tracheal intubation.
In 1926, Sir Magill designed his original U-shaped laryngoscope, a modified version of Hill’s laryngoscope, which itself was also a modified version of Jackson’s laryngoscope.


There was a plethora of laryngoscope blade designs being developed at this time. In 1910 Kirstein advocated for direct laryngoscopic intubation with Kirstein Autoscope, 1941, Robert Miller created laryngoscope with curved tip to hold back epiglottis while in 1943, Sir Robert Macintosh created the curved laryngoscope.
For almost 90 years since Magill designed his laryngoscope and more than 70 years from the introduction of Miller’s and Macintosh’s straight and curved laryngoscopy blades, laryngoscopy essentially remained unchanged. In 1951, Hopkins developed the idea of using a bundle of optical fibers for transporting an optical image and began experiments in 1952. In 1968, Sawashima and colleagues first reported flexible fiberoptic laryngoscopy, however, technology being unacceptable widely, paved way for distal chip technology.
In 1990s with the introduction of rigid fibreoptic endoscopy, Weiss in 1998, modified direct laryngoscopy by incorporating a fibreoptic bundle into the Macintosh blade. A Canadian surgeon, John Pacey, embedded a miniature video chip to a curved non-Macintosh blade, while Berci and Kaplan added the specific DCI Camera Head, with distal light and image fibres (providing optimal illumination and image acquisition) to a standard Macintosh blade. From 2000 onwards, there has been a plethora of different indirect videolaryngoscopes developed.


Videolaryngoscopes also differ in the method of display of the laryngeal view – some have an integrated camera that records images and displays them via a fibreoptic bundle attached video screen, while others use an external video camera that is connected to the scope and an external video screen.

Snow had developed the FM covering both the nose and the mouth in 1847 by adapting the soft nose–piece and mouthpiece used by Francis Sibson (London, 1814 to 1876) to administer ether. It had a symmetrical design, soft material on the edge to fit the face contour, and inspiratory and expiratory valves incorporated in a body made of pliable sheet lead. Replacing ineffective mouthpieces and nares blockers, the FM became the iconic tool of the anesthetist.
Clover’s valveless FM, used with nitrous oxide, was made of sheet lead covered with leather easily molded to the face and edged with india-rubber tubing filled with air or water to create an airtight seal. In the United States, the first FM was patented by Lewis Roper (Philadelphia) in October 1848. It was attached to his inhaler and “shaped to fit closely over the mouth and nose.”
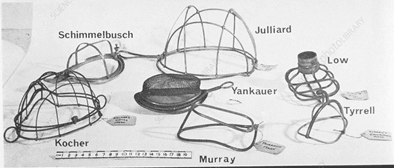
The Schimmelbusch mask is an open breathing system used only for delivering an anesthetic. The device was invented by Curt Schimmelbusch in 1889, and was used until the 1950s (though it is still applied in some developing countries). The device consists of a wire frame which is covered with several beds of gauze and applied to the patient’s face over the mouth and nose. Many scientists, like Yankuer, Tyrell, Julliard have developed anaesthetic FM for ether / ethyl chloride anesthesia.
Many 19th and early 20th Century anesthesia masks were made of metal or of celluloid, and had a detachable rubber rim that could be inflated for a better seal. Throughout the 20th Century, rubber masks were associated with anesthesia machines. The way is now open for the new silicone masks are made of medical grade silicone because this is generally considered the material of choice for its superior ability to conform to the patient’s anatomy.
One of the most important airway gadget which has come the unconditional, unequivocal component for the administration of inhalational anesthetics is the endotracheal tube.
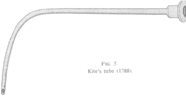
In 1754 Pugh created his ‘air pipe’ but not widely accepted due to instances of traumatic insertion. Charles Kite, a surgeon, was credited in 1788 with saving many from drowning in the Thames using a curved metal cannula blindly introduced into the trachea. In 1807, Chaussier, a physician to the Maternite de Paris, created his own curved metal cannula with a sponge collar near the tip to ensure a tight fit.
In 1880, Macewin created his orotracheal tube with a sponge collar to prevent aspiration, which was introduced orally by touch.

He was also the first to give anesthetic through orotracheal tube. O’Dwyer gained fame for using metal laryngeal tubes in cases of diphtheric croup in 1887. He improved on his design and added a conical end to his tubes for an airtight seal. The end of 19th century marked the first to use inflatable cuff attached to an orotracheal tube by Eisenmenger in 1893.

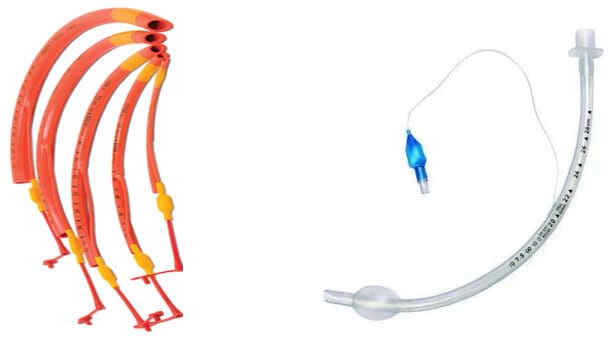
The beginning of the 20th century a malleable tube from rubber and wire to help prevent traumatic insertion was created by Franz Kuhn in 1900. Rowbotham created a wide bore tube with a laryngeal cuff and Magill follows suit with a widebore tube with a tracheal cuff during the World War I (1914-18). These tubes were sealed using pharyngeal sponges with hand-sewn gauze pull strings. The detachable inflatable cuff had been introduced by Trendelenburg, it had fallen out of favour. Guedel (1928) and Waters (1931) reintroduced the inflatable cuff to Magill’s rubber tube and are credited with starting a period of ETT design. Their first cuffs were made from the fingers of rubber gloves and from rubber condoms. Later, they designed cuffs from rubber dental dams that were shorter, 1.5 inches long, and designed to sit below the vocal cords. As polymer technology advanced, a disposable polyvinyl chloride (PVC) tube with a high-pressure low-volume cuff was introduced in 1968. As the high-pressure low-volume cuff became recognized as a problem, manufacturers introduced an HVLP PVC-cuffed ETT in the 1970s, which has become the standard ETT in use today. All tubes have a standard adapter, standardized external diameter of 15 mm, that allows a variety of respiratory or anesthesia equipment to be attached to the tube.
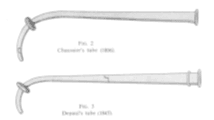
In 1932, Gale and Waters create Endobronchial tubes first used for anesthesia. The tube was rubber and molded in hot water. But, Magill is credited for the development of more stable endobronchial tubes with cuffs (1936). Magill (1936) designed right-sided and left-sided endobronchial tubes with cuffs. Carlens (1949) designed a double-lumen tube (DLT) for spirometric studies, but Bjork used it during thoracic surgery to prevent spillage of contaminated secretions from one lung into the other. Their tube contained a carinal hook to help properly position the left-sided endobronchial tube. Robertshaw (1962) introduced a modified red rubber DLT with right-sided and left-sided versions and a larger internal diameter but without a carinal hook Newer DLT models are similar to the Robertshaw tube except they are made of PVC, have HVLP cuffs, and contain radiopaque markers.

Named after the 3 inventors Ring, Adair, and Elwyn, the RAE ETT was introduced in the 1970s. It is a preshaped orotracheal or nasotracheal tube designed to keep the ETT and breathing circuit away from the surgical field.

For laser surgery, it was not until 2010, 4 specially designed laser-resistant tubes were recommended – Xomed Laser-Shield II , the Sheridan Laser-Trach ETT, the Rusch Lasertubus ETT and the Mallinckrodt Laser-Flex.
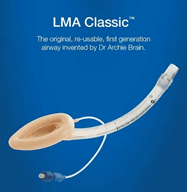
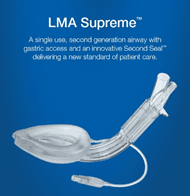
Among the various extraglottic devices, the laryngeal mask airway (LMA; LMA North America, San Diego, CA) was one of the first extraglottic airways (EGA) invented by Dr. Archie Brain in 1981. As known, it has a mask which fits into the supraglottic area without creating trauma caused by endotracheal intubation. Since, its inception now over three decades, designs of extraglottic devices has technologically and rheological improvised and have graduated from first generation to third generation. Specialized LMAs for specific surgical procedures and Various other extraglottic airways like Esophageal Tracheal Combitube, Laryngeal Tube, I-Gel, Air-Q, Laryngeal Mask Airway Fastrach, and the Supraglottic Airway Laryngopharyngeal Tube (SALT) are in the foray.
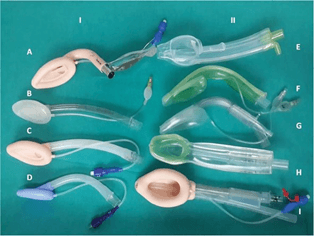
- Extraglottic devices with airway tube only: (A) intubating laryngeal mask airway (B) LMA Unique, (C) classic LMA and (D) disposable laryngeal mask (Romsons).
- Extraglottic devices with both airway and drain tube: (E) Baska mask, (F) Ambu AuraGainTM, (G) LMA SupremeTM, (H) i-gel and (I) ProSealTM laryngeal mask airway.
Patient Monitoring Systems: People have been monitoring the vital signs of others since the dawn of mankind, using various methods to track heart rate, body temperature, respiratory rate, and arterial blood.
The publication of “Pulse-Watch” by Sir John Floyer in 1707 that the first scientific report pertaining to the pulse rate came to light. Ludwig Taube published the first-ever plotted course of fever in a patient circa 1852, adding respiratory rate to the list of human vital signs trackable at the time. Subsequent improvements in the thermometer and clock solidified the heart rate, respiratory rate and body temperature as the standard vital signs monitored by medical professionals of the time.
In 1896 the first ever ‘sphygmomanometer’ (blood-pressure cuff) was introduced to the medical world. Seven years later, in 1903, Willem Einthoven invented the string galvanometer for measuring the ECG – and invention that won him the 1924 Nobel Peace Prize in physiology.
In 1943: Claude Beek first performed electrical defibrillation in the operating room, and began monitoring and clinical application of ECG. Zoll in 1952, introduced cardiac pacing for the first time and led to the advent of external defibrillators in 1956. By 1960s, Continuous bedside ECG monitoring was into patient caring. The 1970s saw the emergence and clinical application of the Swan-Ganz pulmonary artery floating catheter, the introduction of hemodynamic monitoring (invasive pressure, cardiac output, etc.) Thus, greatly promoting medical standards and scientific research. At the same time, Clinical application of continuous non-invasive blood pressure monitoring technology was ensuing.
Due to the wide application of microprocessors and fast electronic systems, the monitoring parameters ECG, SPO2, NIBP, TEMP integrated into monitors were used in clinical applications. The development of second-generation guardianship. In subsequent developments, cardiac output and EtCO2 monitors have also been developed and used especially in ICU, CCU, and anaesthesia.

Photo: Historical Collections, CMHSL, UVa.

Ultrasonography : It was in 1880 when Galton created and produced the apparatus that was able to produce the sound waves of a frequency of 40 hertz. The same year, the brothers Jacques (1856-1941) and Pierre Curie (1859-1906) noted that electricity may be created in a crystal of quartz under mechanical vibrating. This phenomenon was termed the piezoelectric effect.
Dr.Karl Theodore Dussik in Austria in 1942 on transmission ultrasound investigation of the brain provides the first published work on medical ultrasonics. The 1970’s witnessed the widespread use of ultrasound in clinical medicine. Ultrasonography (US) as a means to guide peripheral nerve block (PNB) was first explored by anesthesiologists at the University of Vienna in the mid-1990s. Although radiologists had made use of ultrasound technology, the application of this imaging modality for PNB was novel at that time. Now, unequivocally, one of the most important gadgets in the armamentarium of an anesthesiologist and intensivist.
Nerve locators: In 1962, Greenblatt and Denson devised a portable transistorized nerve stimulator which stimulated further use of nerve stimulators in regional anaesthesia. This equipment was still expensive and not readily available. Finally, in 1969 Wright reported the Block- Aid monitor for nerve blocks but the use of nerve stimulation became widespread in the 1990s. Peripheral nerve blocks were traditionally performed using a technique in which subjective paresthesias were intentionally elicited.
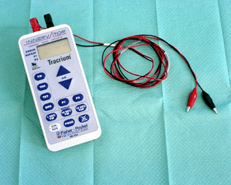
Nerve stimulators: In 1949, Prof W. Mushin reported clinical studies with the drug gallamine. These were performed in volunteers and again mechanically assessed depression from ‘normal/baseline’ was recorded. A dynamometer was constructed in which a pointer moved over a graduated scale and showed ‘flexing power’, power to contract the rectus abdominis muscles etc.
In 1954 Hanquet used needle electrodes in the upper arm of anaesthetised patients and recorded twitches produced in the third finger. In 1955, Mapleson and Mushin from Cardiff described the direct stimulation of motor nerves and recorded muscle activity distally. Over the next three decades, various modes of monitoring were incorporated into various neuro-muscular monitors operating on different principles.

Parallel to the evolution of gadgets designed, redesigned and invented for provision of safe general anaesthesia, regional anaesthesia evolved too.
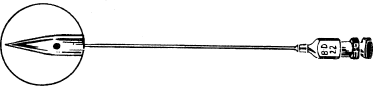
Corning developed his own spinal needle and introducer, which he described in the New York Journal of Medicine. The needle was made of gold or ‘platina’. The cannula was flexible, with a needle stop and a set screw to fix the needle at the correct depth once the subarachnoid space had been entered.
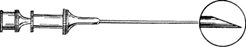
In 1891, Quincke published a paper describing a standardised technique of lumbar puncture for the release of cerebrospinal fluid (CSF) for diseases associated with increased intracranial pressure. He used a needle of which was a sharp, bevelled, hollow needle.
The next major development in the history of spinal anaesthesia was the work of Augustus Karl Gustav Bier, in 1898. He designed a larger bore needle that needed no introducer. The Bier spinal needle was 15G or 17G, with a long, cutting bevel and a sharp point.
Bainbridge described a needle in 1900 that was attached to a metal syringe. It had a small circular hub, a short, sharp cutting bevel and a stylet with a matching bevel. Barker developed a blunt cannula to fit inside the Bier needle that projected 1mm beyond the needle tip.

In 1914, the Quincke–Babcock needle was designed, it was a very successful needle design and became the standard spinal needle for the future.

Gaston Labat needle(1921) and Hoyt needles (1922) were also available. The Greene needle became very popular, especially in obstetrics, due to its low incidence of PDPH, and was the only atraumatic needle in common use until the introduction of the Whitacre needle in 1951.
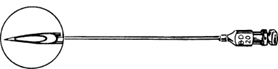
The basic design of Whitacre needle was a success, and is still in common use today with only a few minor modifications to its original design.
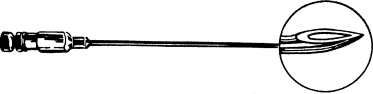
The continuous spinal needle had its problems and was technically difficult to use and keep in position. In 1944, Tuohy used a 15G directional spinal needle through which he passed a nylon ureteric catheter into the subarachnoid space to allow continuous spinal anaesthesia. He advocated to incorporate a ‘Huber tip’, which allowed directional control of the catheter to point cephalad or caudal as required.
We are still striving to perfect the technique of spinal anaesthesia and to find the perfect spinal needle. Perfection may lie in a modified design of the stylet-tipped needle or it may lie in a completely novel design that has not yet emerged.
The first record of an epidural injection is from 1885, when American neurologist James Corning of Acorn Hall in Morristown, NJ used the technique to perform a neuraxial blockade. In 1941, Robert Hingson and Waldo Edwards recorded the use of continuous caudal anesthesia using an indwelling needle,[66] following which they described the use of a flexible catheter for continuous caudal anesthesia in a woman in labor in 1942.[67] In 1947, Manuel Curbelo described placement of a lumbar epidural catheter,[68 Epidural needles are designed with a curved tip to help prevent puncture of the dural membrane
Although Huber intended this needle for IV and tissue injections, Tuohy recognized that the directional point might facilitate placement of spinal catheters (1945). Further, Tuohy added a stylet, thereby hoping to further decrease the risk of skin plugging. But it was Curbelo, not Tuohy, who realized how the directional needle might facilitate the placement of epidural catheters.
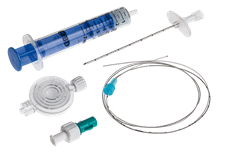

The use of plastic catheters was first described by Flowers et al in 1949. The first polymer (plastic) was polyethylene, which had been introduced as biomaterial for epidural catheters. This material was soon replaced by polyvinyl chloride because of its low melting point, which, similar to the lacquered silk catheters, made it prone to swelling and deformity with sterilization. More recent polymers are nylon, Teflon, polyurethane, and silicone, which have stood the test of time well. The use of these materials enabled manufacturers to produce a thin, yet kink-resistant, catheter with desirable stiffness and tensile strength.
The first documented combined spinal epidural (CSE) procedure with placement of an epidural catheter was performed in 1979 by Curelaru. Over the last 3 decades has gained immense popularity.
Salutations to the great minds and their unrelenting efforts of our forefathers, we should be thankful to be born in this century. The sojourn to perfection is hence on, for the base is well built.
References:
- Markel H. The painful story behind modern anesthesia. PBS NewsHour, Health 2013. Oct 16, 2:49 PM EDT
- Gurudutt CL. The Basic Anaesthesia Machine. Indian J Anaesth. 2013 Sep-Oct; 57(5): 438–445.
- Srivastava U. Anaesthesia gas supply: gas cylinders. Indian J Anaesth. 2013;57(5):500-506. doi:10.4103/0019-5049.120147
- Wood Library-Museum of Anesthesiology (woodlibrarymuseum.org)s
- Pablo Romero-Ávila, Carlos Márquez-Espinós, Juan R. Cabrera Afonso. Historical development of the anesthetic machine: from Morton to the integration of the mechanical ventilator. Brazilian Journal of Anesthesiology (English Edition) Volume 71, Issue 2,2021, Pages 148-161, ISSN 0104-0014 ,https://doi.org/10.1016/j.bjane.2021.02.017.
By Dr. Soma Cham
MD (Anesthesiology)
Ass. Prof. Anaesthesisology


