
Investigations in case of Fever

Consultant Pathologist
MD (Pathology)
Fever is the most common presenting symptom of a varied group of
diseases.
Hence it is important to develop a rational, minimally invasive,
economical approach for investigations of fever resulting in most appropriate
management of the patients.
Broadly the approach will differ depending on the age, history,
localizing signs and duration of fever.
This is review article compiling approach to both pediatric and adult
patients.
Children under 6 weeks of age, any fever (i.e. > 38° C)
This is a high risk group, with bacterial infection in approximately 15% and
the possibility of rapidly progressive disease.
Full sepsis work up is necessary including:
- CXR
- CBC
- Blood cultures
- CSF
- Urine (bladder aspirate or catheter)
A dip stick screen on a bag urine specimen will miss some UTIs and is not
adequate since UTIs are both more common and more serious in this age group. It
is preferable to obtain a definitive urine specimen (bladder aspirate or
catheter) immediately as part of the general sepsis screen to allow rapid
institution of antibiotic therapy in sick infants.
Test for hypoglycaemia in these children as soon as possible.
Children 6 weeks to 3 months of age, any fever (i.e. >38° C)
The risk of bacterial infection in this age group is around 6%
If the infant looks unwell:
- CXR
- CBC
- Blood culture
- CSF,
- Urine (CSU or clean catch)
Perform full sepsis screen:
If the child looks well and feeding is satisfactory:
- Blood culture
- Urine (CSU or clean catch sent to lab)
- CXR if indicated by respiratory signs (grunting, tachypnoea)
Children 3months to two years of age, fever >38.9° C
Decisions regarding investigation and management are based on the child’s
history and examination findings, with particular focus on risk factors for
serious infection, early signs of cardiovascular or respiratory compromise and
the overall appearance and behaviour of the child. Investigations contribute
only a small amount of additional information.
- There is a clear clinical focus of infection in a child
who appears well (alert, responsive and undistressed):
No laboratory investigation is usually necessary. - The child has any of the following; reduced conscious level,
poor perfusion, a petechial rash, signs of cerebral irritation, or just
“looks very sick”:
Full sepsis work up:- CXR
- CBC
- Blood culture
- CSF (unless contraindicated)
- Urine
- The child who has a fever without clinical focus, who is not
severely unwell.
These children have a rate of bacteraemia of ~ 2%, mostly Strep. pneumoniae.
The majority of these cases resolve spontaneously.
CBC and CRP are not useful in determining the risk of bacterial sepsis in a
child presently acutely with fever.
All require screening for a UTI. The prevalence of UTI in this age group
with fever and no clinical focus is 2-5%. It is the most commonly missed
bacterial diagnosis. Diagnosis is challenging as the clinical presentation
tends to be non specific. A bag specimen screened by dipstick is acceptable
in this age group, however a definitive specimen (CSU) is required if the
dipstick is positive for either nitrites or leucocytes. Do not send bag
urine specimens to the laboratory. A child with unexplained persistent fever
or history of UTIs in the past should always have a urine sample obtained.
Consider blood culture in the more unwell child
Chest x ray and CSF specimen should be obtained if indicated by history and
examination. Children who have received prior antibiotics are more likely to
require a CSF specimen despite lack of specific meningeal signs.
Lab Score
The “Lab-score” combining C-reactive protein, procalcitonin and urine
dipstick results has recently been derived and validated as an accurate tool for
predicting severe bacterial infections (SBIs) in children with fever without
source. In well-appearing infants with fever without source, the Lab-score seems
a more useful tool for ruling in, rather than ruling out, SBI. Its accuracy for
IBI (Invasive Bacterial infections) prediction was unsatisfactory.
Evaluation of the Adult Patient with Fever
The initial approach to the patient presenting with fever should include a
comprehensive history, physical examination, and appropriate laboratory testing.
In a patient with short fever with no localization, investigation in any form is
not required in the first 3-4 days of illness in the absence of significant
comorbid conditions like diabetes, cardiac illness, renal disease , liver
disease, old age ,etc. If the illness does not resolve within 4 days then the
basic investigations will be
- Hb%, PCV, Total count, platelet count.
- Urine routine
- RBS
- creatinine
- CPK-Total
- Smear for malarial parasite
- Blood culture
- AST and ALT
Other investigations like ultrasound of abdomen, complete liver function
tests. Routine CXR in the absence of clinical findings or comorbid illness is
not required. Similarly tests like Widal , Ig M ELISA for Dengue , IgM ELISA for
Leptospirosis, other antibody based test may be advised but need to be
interpreted in clinical context.
The following are the findings in the initial investigations which may point towards a particular etiology.
Dengue –
Increased Hb% and PCV , thrombocytopenia and polyserositis[ pleural effusion,
ascites] are diagnostic for dengue .Deranged liver functions can also occur but
are not specific for dengue. Often IgM ELISA for dengue is requested. In a
patient who has all the above mentioned clinical/ lab features, a negative IgM
does not negate the diagnosis. On the other hand if none of the clinical/ lab
features of dengue are present in a patient but IgM for dengue is positive it
does not indicate a diagnosis of dengue.
Malaria –
Anemia, thrombocytopenia, elevated creatinine and deranged liver functions [
hemolytic, hepatitic and cholestatic pattern can occur] may suggest malaria.
However, parasite identification is the definitive indicator of malarial
infection. QBC has a better yield than smear in identifying the parasite
especially among less experienced lab personnel.Tests identifying plasmodium
lactate dehydrogenase [ OPTIMAL] can also be used to identify malarial
infection. This latter test is probably of more value in centres where lab
personnel are not experienced to identify the parasites in peripheral blood.
Further, parasite may escape detection in patients with complicated malaria
due to a phenomenon called visceral pooling. This occurs due to sequestration of
malarial parasites [ often falciparum species] in viscera like liver, spleen,
renal and cerebral blood vessels. Hence patients have all lab features of
complicated malaria except the parasite in blood .
Leptospirosis –
Increased CPK-Total, elevated creatinine and deranged LFT may suugest
leptospirosis. Clinicians should have high suspicion for leptospirosis during
monsoons. However all these investigations can be normal in anicteric
leptospirosis. IgM for leptospirosis can be done; however it is only supportive
and not diagnostic.
Enteric Fever –
Leucopenia and mildly deranged LFT may occur in enteric fever. However a
similar picture can occur in many non-specific viral infection. Blood culture in
the first week of illness and stool culture in the second and third week of
illness is the gold standard in the diagnosis of enteric fever. Blood Widal has
high false positivity and has been consistently shown to have poor clinical
value in the diagnosis of enteric fever.
Diagnosis of Fever of Unknown Origin
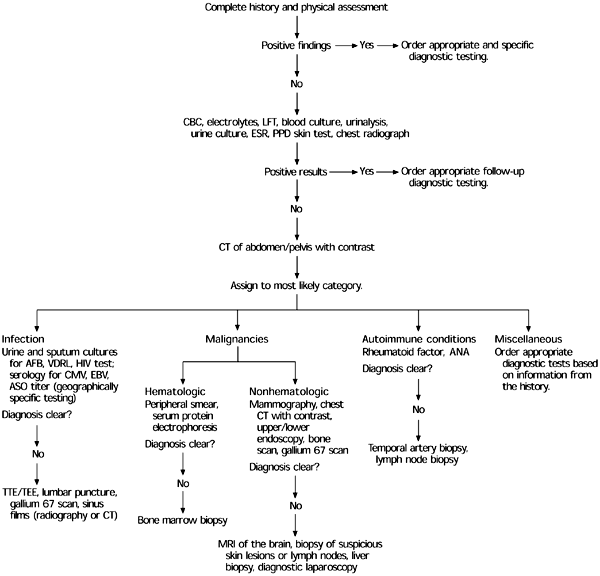
FIGURE 1.
Algorithm for the diagnosis of fever of unknown origin. (CBC = complete blood count; LFT = liver function test; ESR = erythrocyte sedimentation rate; PPD = purified protein derivative; CT = computed tomography; AFB = acid-fast bacilli; HIV = human immunodeficiency virus; CMV = cytomegalovirus; EBV = Epstein-Barr virus; ASO = antistreptolysin-O antibodies; ANA = antinuclear antibody; TTE = transthoracic echocardiography; TEE = transesophageal echocardiography; MRI = magnetic resonance imaging)
The preliminary evaluation helps in the formulation of a differential
diagnosis and guides further studies that are more invasive or expensive. These
preliminary investigations should include a complete blood count, liver function
test, erythrocyte sedimentation rate, urinalysis, and basic cultures. Simple
clues found during initial testing often will guide the clinician toward one of
the major subgroups of FUO. The decision to obtain further diagnostic studies
should be based on abnormalities found in the initial laboratory work-up and not
represent a haphazard use of costly or invasive modalities.
Skin testing for tuberculosis with purified protein derivative (PPD) is an
inexpensive screening tool that should be used in all patients with FUO who do
not have a known positive PPD reaction. However, a positive PPD reaction alone
does not prove the presence of active tuberculosis. A chest radiograph also
should be obtained in all patients to screen for possible infection, collagen
vascular disease, or malignancy. If this initial assessment does not disclose
the source of fever, more specific investigatory techniques, such as serology,
sonography, computed tomography (CT), magnetic resonance imaging (MRI), and
nuclear medicine scanning should be conducted, based on clinical suspicion.
Laboratory Diagnosis (TABLE 1)
| Test | Sample | Findings | Possible diagnosis |
| Complete Blood Count(CBC) | Blood | Anemia Blasts Lymphocytosis(with atypical cells) Leukocytosis (with increase in bands) Parasites on smear (Repeated examinations necessary) |
Suggest serious underlying disease Leukemia/Preleukemia Herpesvirus infection Occult bacterial infection Malaria/Spirochaetes |
| Urinalysis | Pus cells Malignant cells |
UTI Urinary tract tumours |
|
| Serum Chemistry | At least one of LFT is abnormal Other chemistry tests |
Liver disease/Disease affecting Liver Rarely contribute to diagnosis |
|
| Cultures | Urine culture(done routinely) Maximum 6 sets of Blood cultures Sputum/stool Fluids/BM/LN/CSF |
+ + + + |
To rule out UTI Aerobic/Anaerobic infections suggesting Pulm/GI disease for bacteria/mycobacteria/fungi |
| Serology | Paired serum samples | 4 fold rise in antibody levels | Brucellosis,CMV,EBV,HIV, Amebiasis Toxoplasmois, Chlamydia |
| Pprotein electrophoresis (SPEP) | Serum | e.g. paraprotienemias | atrial myxoma, SLE flares, and lymphomas. |
| Ferritin levels | Serum | Raised | FUO due to malignancies, SLE flare, and adult Still disease |
| ANA,RF,TSH, | Serum | SLE,RA,Thyroiditis,Hyperthyroidism,GCA,PMR | |
| ESR | Blood | > 60 mm/h | GCA, PMR |
| Biopsy | Involved tissue e.g; lymph node,BM | Specific infections, neoplastic conditions |
Abdominal sonography, pelvic sonography, or CT scanning should be performed
early in the diagnostic process to rule out such common causes of FUO as
intra-abdominal abscess or malignancy, depending on the primary evaluation This
testing, including directed biopsies, has greatly reduced the need for more
invasive operative studies.
MRI should be reserved for clarifying conditions found through the use of
other techniques or when the diagnosis remains obscure. The use of
radionucleotide scanning, such as gallium 67, technetium Tc 99m, or
indium-labeled leukocytes, is warranted for detecting inflammatory conditions
and neoplastic lesions that often are underdiagnosed by CT scans; however, these
tests tend not to detect collagen vascular disease and other miscellaneous
conditions (Table 2).
Diagnostic Imaging in Patients with FUO (TABLE 2)
| Imaging | Possible diagnoses |
| Chest radiograph | Tuberculosis, malignancy, Pneumocystis carinii pneumonia |
| CT of abdomen or pelvis with contrast agent | Abscess, malignancy |
|
Gallium 67 scan |
Infection, malignancy |
|
Indium-labeled leukocytes |
Occult septicemia |
|
Technetium Tc 99m |
Acute infection and inflammation of bones and soft tissue |
| MRI of brain | Malignancy, autoimmune conditions |
| PET scan | Malignancy, inflammation |
| Transthoracic or transesophageal echocardiography | Bacterial endocarditis |
| Venous Doppler study | Venous thrombosis |
FUO = fever of unknown origin; CT = computed tomography; MRI = magnetic
resonance imaging; PET = positron emission tomography.
Endoscopic procedures may be helpful in the diagnosis of disorders such as
inflammatory bowel disease and sarcoidosis. The newest diagnostic technique in
the evaluation of the patient with FUO is positron emission tomography (PET).
This modality appears to have a very high negative predictive value in ruling
out inflammatory causes of fever. However, because of its limited availability
it is too early to determine if PET scans will prove to be a useful diagnostic
tool in the evaluation of these patients. More invasive testing, such as lumbar
puncture or biopsy of bone marrow, liver, or lymph nodes, should be performed
only when clinical suspicion shows that these tests are indicated or when the
source of the fever remains unidentified after extensive evaluation. When the
definitive diagnosis remains elusive and the complexity of the case increases,
an infectious disease, rheumatology, or oncology consultation may be helpful.
References:
- Approach to the Adult Patient with Fever of Unknown Origin
ALAN R. ROTH, D.O., and GINA M. BASELLO, D.O., Jamaica Hospital Medical
Center, Mount Sinai School of Medicine Family Practice Residency Program,
Jamaica, New York
Am Fam Physician. 2003 Dec 1;68(11):2223-2229. - Diagnostic Performance of the Lab-score in Predicting Severe and Invasive
Bacterial Infections in Well-appearing Young Febrile Infants
Silvia Bressan, MD, Borja Gomez, MD, Santiago Mintegi, MD, PhD, Liviana Da
Dalt, MD, Daniel Blazquez, MD, Izaskun Olaciregui, MD, Mercedes de la Torre,
MD, Miriam Palacios, MD, Paola Berlese, MD, Aitor Ruano, MD
Pediatr Infect Dis J. 2012;31(12):1239-1244. - Neonatal Sepsis Workup
Author: Ann L Anderson-Berry, MD - FEVER IN CHILDREN
Dr Wong Chin Khoon, Consultant, The Children’s Medical Institute, National
University Hospital - FEVER – INVESTIGATION & MANAGEMENT
Author: Dr Richard Aickin, Dr Mike Shepherd, Service: CED Editor: Dr Raewyn
Gavin Date Reviewed December 2009 - Fever of Unknown Origin
Author: Kirk M Chan-Tack, MD; Chief Editor: Burke A Cunha, MD - Approach to short fever- Management
Dr.M.Emmanuel Bhaskar, Specialist in Internal Medicine, Chennai , India

