
Labour Analgesia

Dr. Manisha Shembekar
Anaesthesiologist, Nagpur
Labour pain is the worst pain that a woman experiences during her lifetime. It is not just pain but a complete physical, mental and emotional assault on her body. According to American Society of anaesthesiology, in the absence of contraindication, maternal request is a sufficient medical indication for pain relief during labour.
Delivery of the infant into the arms of a conscious and pain free mother is one of the most exciting and rewarding moments in medicine–Moir
History- In 1847, Dr. J.Y. Simpson was the first one to administer ether to a woman during childbirth. Later in 1853, Dr. John Snow gave chloroform to Queen Victoria for the birth of her eighth child, which popularized pain relief in labour.
Ideal Obstetric analgesic should be safe for mother and the baby, easy to administer, should not interfere with the process of labour and should be flexible to changing demands of labour.
Stages of labour-
- First stage is from the onset of true labour pains to full cervical dilatation
- Second stage is from full cervical dilatation to delivery of baby.
- Third stage is delivery of placenta and membranes.
- Fourth stage of observation.
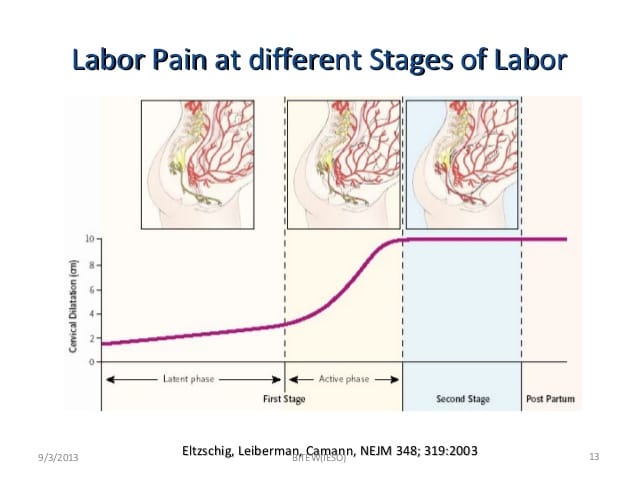
Pathophysiology of labour pain–
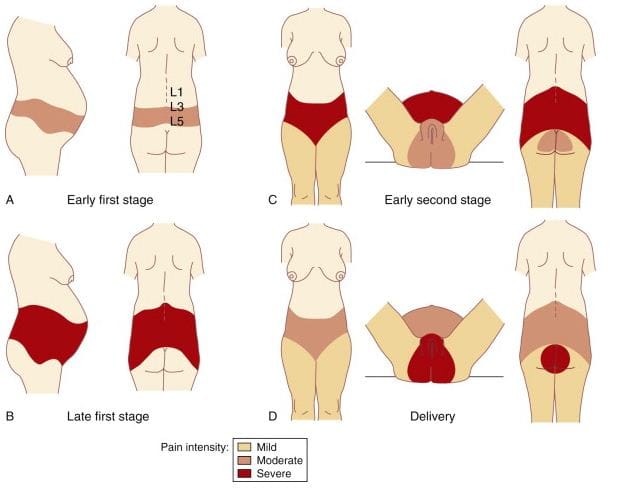
Pain in first stage of labour- arises from uterine contraction and cervical dilatation and is referred to cutaneous branches of T10- L1 dermatomes.
Pain in second stage of labour is caused by distension of perineum by the presenting part, stretch on bladder, urethra, rectum and is referred to lower lumbar and sacral segments. Pain is carried by A delta and C fibres.

Advantage of labour analgesia– it causes reduction in the release of maternal catecholamines, prevents hyperventilation and hypocarbia and prevents shift of oxyhaemoglobin dissociation curve to left. Thus pain relief during labour has advantages for mother as well as baby.
Various methods have been tried and described.
Prepared Child birth– This method was described by Grantly Dick-Read. It involves educating the mother about anatomy of pelvis and physiology of labour and preparing her for the forthcoming event of labour.
Muscle relaxation and Breathing techniques was described by Lamaze. Would be mothers are taught about breathing techniques during labour which helps them face labour pain and child birth.
Psychoprophylaxis and hypnosis have been tried by Lamaze. Other methods like massage, warm bath and use of heating pads have been tried.
Acupuncture-insertion of needles at specific points helps relieve pain. During first stage of labour points in hands, legs, lower abdomen, sacrum and feet are used. In second stage points in upper inner thigh and perineum are used.
TENS– Trans electrical nerve stimulation during labour was also described as one of the methods of analgesia. Electrical impulses are applied to skin via electrodes. For first stage, electrodes are applied to T10-11 on either side of spinous process. For second stage electrodes are placed over S2-S4.

Pharmacological methods-
Inhalational analgesics-
Gaseous- Nitrous oxide
Volatile – Enflurane
Isoflurane
Desflurane
Sevoflurane
- Nitrous oxide was introduced in 1880 by Kilkovicz while Dr. R.J. Minritt developed a system for its premixing in 1933. Tunstall demonstrated that under pressure of 2000 psi oxygen would dissolve nitrous oxide in the gas phase which behaves as a single gas. Since then, it is marketed by British Oxygen company as Entonox.
Certain precautions should be taken prior to using Entonox cylinders. They should be stored horizontally for 24 hours before use. Smaller cylinders should be stored at temperature more than 10 degrees before use. They should be gently inverted three times before use to ensure adequate mixing of gases.Entonox can be self administered by the patient when she feels the contractions. It takes 15-20 minutes to achieve effective arterial concentration and about a minute for maximum analgesic effect. During second stage, the parturient takes 3-4 deep breaths at the onset of contractions followed by pushing.
Side effects-patient may have nausea, vomiting, drowsiness and disorientation. Patient tends to hyperventilate in order to achieve better analgesia. This may cause shift of the oxyhaemoglobin dissociation curve to the left, thereby causing reduction in the uterine blood flow and fetal oxygenation.
However, nitrous oxide is the safest inhalational agent with no organ toxicity been reported. - Enflurane and Isoflurane– these inhalational agents have been uded in subanesthetic doses either alone or in combination with nitrous oxide. Both enflurane 1% and isoflurane 0.75% have faster rates of uptake and provide good analgesia during first stage of labour. In the second stage continuous inhalation has provided satisfactory analgesia.
Disadvantages are drowsiness and theoretical risk of renal failure due to fluoride ions. However, in subanesthetic doses, there is no depressant effect on neonate nor increase in blood loss.
Desflurane– Due to its low blood gas coefficient, it allows rapid onset and offset of action. It provides effective analgesia comparable to Nitrous oxide. Patient may have amnesia after its use.
- Sevoflurane– Sevoflurane has low blood gas coefficient of 0.65. Hence uptake and elimination of the agent is rapid. It has a pleasant odour and is less irritant to the respiratory tract. Can be given as 0.8%. Disadvantage is it causes pollution of labour suit and airway reflexes may be lost.
These agents did not gain much popularity because of exposure of health care workers to high concentrations of inhalational agents.
Systemic analgesics- they have a certain advantage of ease of administration. Anesthesia personnel is not required. They are inexpensive and require minimal monitoring. Moreover, rate of complications is very low.
Disadvantage is inadequate pain relief, delayed gastric emptying, nausea, vomiting, respiratory depression. They may cause neurobehavioural changes in the fetus, beat to beat variability may be lost.
- Opioids-
Pethidine– it is the most popular drug in Obstetric practice due to its lipophilicity and potent analgesic property. It can be given 25-50 mg IV or 50-100 mg IM. The peak effect occurs within 10 minutes of IV administration and 45 minutes of IM administration. Pethidine causes increase in contractility of body of uterus and reduced contractility of the cervix, thus facilitating cervical dilatation and thereby labour. However respiratory depression in the neonates is seen if delivery takes place within 2-3 hours of administration of the drug.
Fentanyl– It is rapidly acting and has shorter duration of action. It is highly lipid soluble and does not have any active metabolites. It can be given IM 50-100mcg. Analgesia begins in 7-8 minutes, peaks at 30 minutes and lasts for 60 minutes. After IV administration onset of analgesia is within 3-5 minutes and lasts for 30-60 minutes.
Remifentanyl– it can be used as patient controlled IV anesthetic agent PCIVA. Can be given in 0.2-0.5mcg/kg with 2 minute lockout interval and no concurrent infusion. Drowsiness and apnea are the common side effects. Oxygen saturation monitoring should be done diligently and there should be access to Naloxone.
Low dose Ketamine analgesia for painless labour
This method has been tried by some clinicians. Antacid prophylaxis is given. Complete preanesthetic evaluation is done. In first stage of labour, bolus dose of Ketamine 10-15mg followed by infusion of 0.5-1mcg/kg/min is given. At the time of crowning, 0.2-0.4mg/Kg can be repeated. Dose should not exceed 100 mg.
Verbal contact with the patient should be maintained. Patient may have restlessness, disorientation, dryness of mouth. Possibility of neonatal depression is there if total dose exceeds 100mg.
Regional Analgesia
It is by far the best technique of providing pain relief during labour without any depressant effect on the neonate and provides satisfactory analgesia to the mother. Moreover, it can provide anesthesia for caesarean section if need arises.
Indications –
- Maternal request
- High risk parturient having hypertension, pulmonary or cardiac diseases. It reduces the catecholamine secretion and hyperventilation which immensely helps to improve the outcome of labour.
- Fetal complications- prematurity or small for date babies have a definite advantage.
Contraindications-
- Patient refusal
- Local infection
- Bleeding disorders
Preanesthetic checkup – A thorough examination should be done prior to initiation of block. The fetal status should be assessed and informed consent should be obtained. Intravenous infusion should be started. All the equipments and drugs for resuscitation should be kept ready. Maternal and fetal monitors should be available.
When should analgesia be initiated?
- Patient should be in active phase of labour i.e. cervical dilatation of 3-4 cm
- Uterine contractions should be regular occurring every 3-4 minutes lasting 35-40 seconds.
- Presenting part should be engaged.
However, analgesia can be started on demand even at 2-3 cm dilatation. Chestnut et al have found that there is no increased incidence of caesarean section even if epidural analgesia is given earlier.
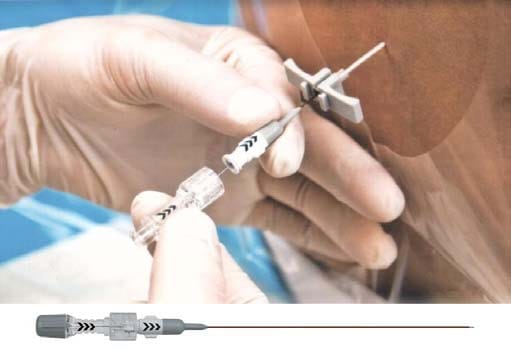
Place epidural catheter in L3-4, L4-5 space, give a test dose of 2ml Xylocaine with adrenaline. Wait to rule out intrathecal injection which will cause dramatic pain relief or intravascular injection causing tachycardia. When epidural placement is confirmed, give a bolus dose.
First dose of Bupivacaine 10-12ml 0.125% with 10 microgram/ml of Fentanyl is given. Ropivacaine 0.125%-0.175% can be given. Advantage of using Ropivacaine over Bupivacaine is less cardiotoxicity, less sensory and motor block.
Subsequent doses can be given intermittently or as continuous infusion. Top up doses can be 5-6 ml 0.125% Bupivacaine with Fentanyl on demand or 45-60 minutes later. Continuous infusion 8-15ml/hour of 0.0625- 0.125% Bupivacaine with 20-25 micrograms of Fentanyl can be started 15 minutes after the initial dose.
PCEA- Patient controlled epidural analgesia can be given as background infusion of 4-6ml/hour and on demand bolus of 3-4 ml with lock out interval of 20 minutes.
Blood pressure should be checked every 1-2 minutes for first 10 minutes and every 5-15 minutes during the infusion.
Check level of sensory and motor block during the top ups.
For perineal analgesia 10-20 ml of local anesthetic may be required.
Oxytocin infusion may be required for augmentation of labour. Second stage of labour may be prolonged during epidural analgesia. Duration of second stage of labour in nullipara without analgesia is 2 hours and in multipara, it is 1 hour. With regional analgesia it may be prolonged by 1 hour in both primi and multiparas. However, with electronic fetal monitoring, this increase in duration of second stage is safe and acceptable.

New continuous infusion devices
Combined Spinal Epidural analgesia
CSE is especially beneficial if request for analgesia is made in later stages of labour when cervical dilatation exceeds 4-5 cm. Advantage is rapid pain relief within 2-3 minutes. Epidural analgesia can be initiated later to provide pain relief throughout labour. Intrathecal Bupivacaine 1-2.5mg with Fentanyl 25 micrograms can be given.
Walking or Ambulatory Analgesia– It is a CSE with low dose intrathecal analgesia with epidural analgesia using low dose opioids and local anesthetics . There is no motor block, no hypotension, better patient satisfaction.
Safe maximum dose of Fentanyl is 200 micrograms and Sufentanyl is 30-50 micrograms .
Monitoring-
Maintain verbal contact with mother. If she complains of dizziness or light headedness inadvertent intravascular injection should be suspected. Numbness in lower extremities followed by hypotension and difficulty in breathing indicates accidental intrathecal injection.
Assess sensory block after each top up dose. Assess motor block by straight leg raising test against resistance. It must be assessed prior to attempt at ambulating.
Continuous electronic fetal heart rate monitoring is preferable until delivery.
Pain assessment– Site and severity of pain before and after every top up must be assessed. During infusions, breakthrough pain must be assessed. Perineal pain in labour is felt in later stages of labour, especially if the epidural catheter is placed in L2-L3 space or above. Sacral spread is encouraged by giving a 25degree head up tilt or addition of Fentanyl to the top-up dose.
Complications –
- PDPH-Accidental dural puncture resulting in postdural puncture headache may occur.
- Trauma – Direct trauma to spinal cord
- Fetal bradycardia
- Hypotension- can occur due to sympathetic block.
- Total spinal anesthesia- rare complication as the concentration of local anesthetic drug used for epidural is low.
Controversial issues-
- Backache –studies have found that there is no increase in incidence of backache after epidural analgesia.
- Rate of cervical dilatation- there was a misconcept that epidural analgesia if given early in labour may slow the progress of labour. More recent studies have failed to confirm this theory.
- Prolongation of second stage of labour-There may be impairment of the urge to push during second stage of labour, there may be inhibition of the Ferguson reflex. Relaxation of pelvic muscles may delay the fetal descent and rotation. Due to availability of electronic fetal monitors, the arbitrary limits of duration of second stage of labour are not important.
- increased incidence of operative delivery-There may be increased incidence of use of forceps or vacuum for delivery due to reduced expulsive efforts of the mother. However, incidence of caesarean section has not increased.
- Urinary retention can occur due to opioids and may require catheterization.
Evaluation of fetus
Assessment of fetus should be done prior to initiation of epidural analgesia and should be continued throughout labour using electronic fetal monitors applied externally. Fetal heart rate can be assessed internally with fetal scalp electrodes. Normal fetal heart rate varies between 120-160/minute. Early decelerations occur with uterine contractions upto 110 per minute. It occurs in second stage of labour due to vagal stimulation. Late decelerationof 20 seconds or more represents uteroplacental insufficiency.

Normal cardiotocograph
Key points
- Epidural analgesia is by far the best method of pain relief described till date.
- Bupivacaine is the best and most commonly used local anesthetic.
- Levobupivacaine and Ropivacaine are safe alternatives.
- Addition of opioids provides excellent analgesia while reducing the dose of local anesthetics.
- Hypotension is one of the side effects which has to be monitored and taken care of by preventing aortocaval compression, preloading and adding vasopressors if required.
- Accidental dural puncture, intravascular injection, total spinal anesthesia are rare complications.
- Patient may experience shivering, pruritus, urinary retention and there may be fetal heart rate variations.
- Maternal and fetal indications are the most important determinants of caesarean delivery and neuraxial block per se does not interfere with the delivery process and does not determine the rate of caesarean section.





